UnitedHealth's Federal Investigation: Implications for Healthcare Sector Stability
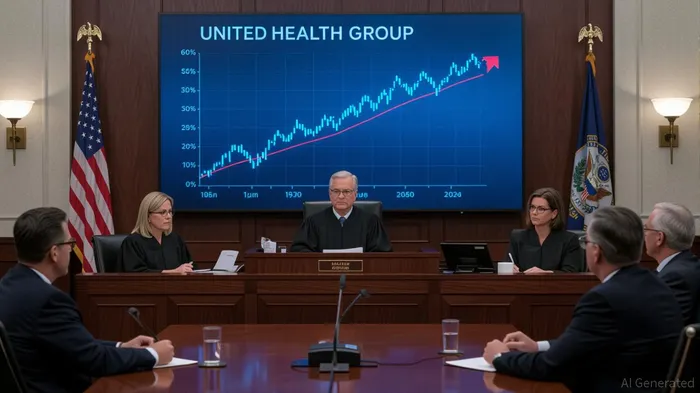
The healthcare sector has long operated in a delicate balance between innovation, profitability, and regulatory oversight. UnitedHealth GroupUNH--, the largest private health insurer in the U.S., now finds itself at the center of a storm that could redefine how investors view risk and valuation in a heavily regulated industry. A federal investigation into its Medicare Advantage billing practices—announced in early 2025—has sent shockwaves through the market, with shares plummeting nearly 4% in premarket trading and the company losing over $288 billion in market value since the beginning of the year. For investors, the question is no longer just about UnitedHealth's fate but whether this saga signals a broader shift in how the sector navigates regulatory scrutiny.
The Investigation: A Catalyst for Sector-Wide Reassessment
The Department of Justice (DOJ) is probing UnitedHealth's Medicare Advantage program, alleging that the company may have inflated diagnoses to secure higher federal reimbursements. This follows a pattern of scrutiny that began in 2021, when the Wall Street Journal revealed that UnitedHealth's practices generated an estimated $8.7 billion in extra payments. The latest probe, however, marks a significant escalation, combining criminal and civil investigations with interviews of physicians about alleged pressure to submit claims for specific conditions.
While UnitedHealthUNH-- has maintained its commitment to compliance and cited independent audits confirming its billing accuracy, the damage to its reputation—and by extension, the sector's stability—is palpable. The company's stock, which had already lost 42% of its value in 2024 amid a cyberattack, CEO murder, and leadership turmoil, now faces renewed uncertainty. For investors, this underscores a critical risk: even the most dominant players in regulated industries are not immune to regulatory overreach or reputational collapse.
Historical Precedents: Financialization, Scrutiny, and Valuation Shifts
To understand the broader implications, consider the historical trajectory of healthcare sector valuation. Over the past two decades, the sector has undergone a profound financialization, driven by regulatory shifts that prioritized shareholder value over community service. From 1998 to 2017, nearly 1,600 hospital mergers reshaped the industry, with consolidation enabling firms to leverage market power and secure higher reimbursement rates. Private equity investments in healthcare, which surged from $5 billion in 2000 to $100 billion in 2018, further entrenched this model, treating hospitals and insurers as tradable assets.
However, this financialization has not been without consequences. Federal investigations into antitrust violations, billing fraud, and patient access issues have repeatedly disrupted valuations. For example, in 2021, a bipartisan congressional inquiry into private equity's role in healthcare revealed that cost-cutting measures under PE ownership often degraded care quality, leading to lawsuits and regulatory pushback. Similarly, nonprofit hospitals' tax-exempt status has come under fire as scrutiny intensifies over their community benefits.
UnitedHealth's case fits into this pattern. Its Medicare Advantage business—accounting for $139 billion in sales in 2024—has become a lightning rod for concerns about profit-driven risk assessment coding and managed care practices. The DOJ's focus on these issues suggests a broader regulatory pivot toward curbing financialization in healthcare, with potential ripple effects on valuation models that relyRELY-- on scale, market power, and risk inflation.
Assessing Risk Exposure: A Sector in Transition
For investors, the key challenge lies in disentangling UnitedHealth's specific risks from the sector's structural vulnerabilities. The company's current crisis highlights three critical areas:
- Regulatory Uncertainty: The DOJ's dual criminal and civil investigations could set a precedent for stricter oversight of Medicare Advantage billing. If penalties or reforms emerge, the entire sector may face higher compliance costs and reduced profitability.
- Market Power vs. Public Trust: UnitedHealth's dominance in Medicare Advantage (35% market share as of 2024) gives it significant leverage, but public backlash over perceived exploitation of federal programs threatens long-term stability. Similar tensions have dented the reputations of other insurers, such as Anthem and Aetna, during past investigations.
- Financialization's Limits: The sector's reliance on financial engineering—whether through private equity roll-ups or aggressive risk coding—may be reaching a breaking point. As regulators and policymakers prioritize affordability over profitability, traditional valuation metrics may become less reliable.
Long-Term Valuation: Navigating the New Normal
Despite the short-term pain, the healthcare sector remains a cornerstone of the U.S. economy. Medicare Advantage enrollment is projected to grow by 10% annually through 2030, driven by an aging population and policy shifts favoring managed care. However, investors must now factor in a new reality: regulatory scrutiny will likely intensify as lawmakers and regulators seek to address rising healthcare costs and inequities.
For UnitedHealth, the path forward hinges on its ability to reconcile its business model with these demands. Its recent third-party audits and transparency initiatives are steps in the right direction, but they must be followed by concrete actions—such as overhauling risk assessment protocols or capping reimbursement incentives tied to inflated diagnoses. Competitors like HumanaHUM-- and CignaCI--, which have faced similar scrutiny, may also need to recalibrate their strategies.
Investment Advice: Prudence in a Volatile Era
In this environment, investors should adopt a cautious, diversified approach. Here's what to consider:
- Sector Hedges: Allocate a portion of healthcare exposure to companies with less regulatory risk, such as those focused on innovation (e.g., MedTech firms) or essential services (e.g., pharmacy chains).
- Valuation Metrics: Rely less on traditional multiples (P/E, EBITDA) and more on qualitative factors like regulatory compliance, community benefit programs, and transparency in billing practices.
- Policy Monitoring: Track legislative and regulatory developments, particularly around Medicare Advantage reforms, antitrust enforcement, and nonprofit hospital oversight.
UnitedHealth's current crisis is a microcosm of the sector's broader challenges. While its stock may recover if the DOJ investigation concludes with manageable penalties, the long-term outlook depends on whether the industry can adapt to a regulatory landscape that prioritizes accountability over profit maximization. For now, the message is clear: in healthcare, as in any regulated industry, stability is a fragile commodity—one that demands vigilance, adaptability, and a willingness to rethink the status quo.
Tracking the pulse of global finance, one headline at a time.
Latest Articles
Stay ahead of the market.
Get curated U.S. market news, insights and key dates delivered to your inbox.

Comments
No comments yet