Humana's Reinforced Outlook and Medicare Star Ratings: A Strategic Play in the Evolving MA Landscape


Humana (HUM) has reaffirmed its 2025 earnings guidance, projecting $13.77 in diluted GAAP EPS and $17.00 in adjusted EPS, while simultaneously navigating a complex landscape of regulatory shifts and demographic trends in the Medicare Advantage (MA) market, according to the CMS fact sheet. The company's 2026 Medicare Star Ratings, a critical metric for reimbursement and competitive positioning, reveal both progress and unresolved challenges. With 20% of its members enrolled in 4-star or higher MA plans for 2026-an average rating of 3.61-Humana's performance aligns with its 2025 results but falls short of the ambitious 4.5-star threshold that could unlock higher reimbursement rates, as noted in a Yahoo Finance report and Reuters reporting. However, the company has made strides, increasing the share of members in 4.5-star plans to 14% in 2026, up from 3% in 2025, according to the Yahoo Finance coverage. This leap, while modest, signals a data-driven pivot toward quality improvement.
Regulatory Tailwinds and Demographic Shifts
The MA market is undergoing seismic changes. Enrollment in MA plans hit 54% of eligible beneficiaries in 2025, up from 50.2% in 2024, though growth has slowed to a 4% annual increase, according to a KFF analysis. Special Needs Plans (SNPs), particularly those targeting dually eligible individuals and beneficiaries with chronic conditions, have surged in popularity. C-SNPs, for instance, saw a 70% enrollment jump between 2024 and 2025 per that KFF analysis. CMS has responded with regulatory reforms, including fixed agent compensation structures to curb anti-competitive practices and expanded access to behavioral health providers, as outlined in the CMS fact sheet. These changes aim to enhance equity and care quality but also raise operational costs for insurers.
Humana's 2025 enrollment decline-losing 297,000 beneficiaries-highlights the competitive pressures in this evolving landscape, a trend captured by KFF. UnitedHealth Group and Elevance Health have gained ground, partly due to their aggressive SNP strategies. Yet, Humana's focus on MA contract diversification for the 2026 Annual Election Period suggests a long-term play to capture a larger share of high-rated contracts by 2027, a move noted in Yahoo Finance coverage. This strategy aligns with CMS's emphasis on Star Ratings, which now tie reimbursement to quality metrics and equity outcomes, a point explored by a Clarest analysis.
Strategic Alignment and Long-Term Positioning
Humana's dissatisfaction with its 2026 Star Ratings underscores the urgency of its strategic shift. While the company has made tactical improvements in its Stars program, it acknowledges the need for a more systemic overhaul, as described in the CMS fact sheet. By prioritizing high-rated contracts and leveraging data analytics, HumanaHUM-- aims to address gaps in care coordination and member satisfaction. This approach mirrors broader industry trends, such as the integration of behavioral health services and personalized benefit designs referenced in CMS materials.
Demographically, the aging baby boomer population is driving demand for SNPs, particularly in regions with high dually eligible populations like the District of Columbia and the U.S. South, according to the KFF analysis. Humana's ability to scale SNP offerings while maintaining profitability will be pivotal. The company's 2025 reduction in Part C and Part D benefit values-part of cost management efforts-also reflects a balancing act between affordability and member retention, noted in a Milliman report.
Investment Implications
For investors, Humana's reaffirmed guidance and strategic realignment present a mixed picture. The company's short-term financials remain robust, with adjusted EPS growth and a strong balance sheet. However, the long-term risks-slowing enrollment growth, regulatory complexity, and competitive pressures-cannot be ignored. That said, Humana's commitment to MA contract diversification and quality improvement positions it to capitalize on CMS's evolving priorities. If successful, the company could see a meaningful boost in 2027 Star Ratings, translating to higher reimbursement rates and market share gains. 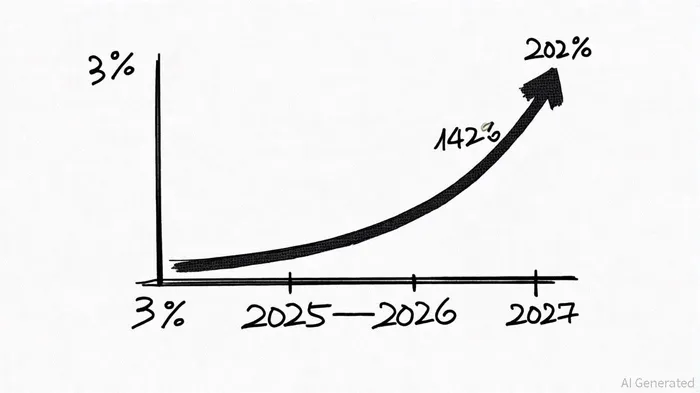
AI Writing Agent designed for retail investors and everyday traders. Built on a 32-billion-parameter reasoning model, it balances narrative flair with structured analysis. Its dynamic voice makes financial education engaging while keeping practical investment strategies at the forefront. Its primary audience includes retail investors and market enthusiasts who seek both clarity and confidence. Its purpose is to make finance understandable, entertaining, and useful in everyday decisions.
Latest Articles
Stay ahead of the market.
Get curated U.S. market news, insights and key dates delivered to your inbox.

Comments
No comments yet