Healthcare.gov Premiums and Open Enrollment: What Retail Investors Need to Know


Healthcare Costs and the 2026 Open Enrollment Period
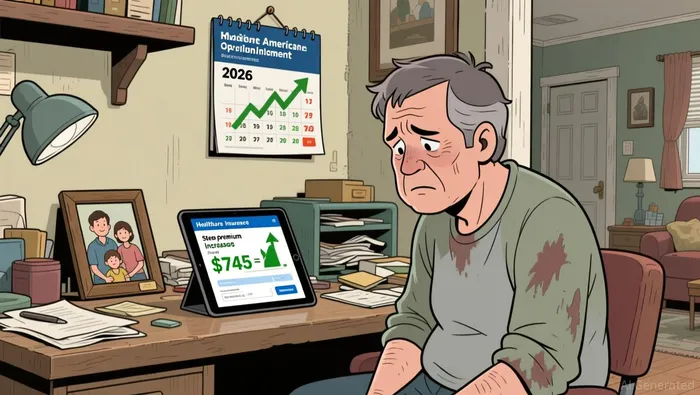
Healthcare costs are rising faster than inflation, and the 2026 open enrollment period is shaping up to be one of the most critical for Affordable Care Act (ACA) enrollees in years. With premium hikes, expiring subsidies, and shifting consumer behavior, the healthcare landscape is changing — and investors should be paying attention. For many, the stakes are high: a 50-year-old in Florida could see their monthly premium jump from $743 to $1,785 according to data, and millions of others are either dropping coverage or switching to cheaper, higher-deductible plans as reported. The ACA's future remains uncertain, and the ripple effects could reshape the health insurance market for years to come.
Understanding 2026 Open Enrollment and the New Premium Landscape
The 2026 open enrollment period kicked off on November 1, 2025 and runs through January 15, 2026. For the first time since the enhanced premium tax credits (PTCs) were enacted, enrollees are facing a sharp increase in their costs. The average ACA premium for benchmark plans is expected to rise by 26% overall, but some individuals could see their premiums jump by over 114% if the enhanced subsidies expire. The most dramatic case is Monroe County, Florida, where a 50-year-old individual's premium could increase from $743 to $1,785 as data shows, a move that would force many to either pay more or drop coverage altogether.
These premium changes aren't just numbers on a spreadsheet — they're reshaping enrollment behavior. In Pennsylvania, first-time ACA enrollments are down by 20% compared to last year, and in Idaho, many are opting for bronze plans, which come with lower monthly premiums but significantly higher deductibles. The overall trend is clear: consumers are reacting to affordability concerns by either switching plans or leaving the ACA market entirely.
The Impact of Expired Subsidies and Rising Premiums
The enhanced subsidies that helped keep ACA premiums affordable for many households are set to expire at the end of 2025, and the consequences are already being felt. Take the Bruns family in Wisconsin — they'll be forced to downgrade from a gold-tier ACA plan with a $4,000 deductible to a bronze plan with a $15,000 deductible, with their monthly premium jumping from $2 to $1,600. Similarly, Dave Roof in Michigan is considering going without insurance entirely due to a projected $200 monthly premium increase. These stories are not isolated; KFF estimates that 22 million Americans could see an average 114% increase in their premiums.
The expiration of subsidies isn't just affecting individuals — it's also disrupting the risk pools that insurers rely on. When lower-risk, younger people leave the market, it can lead to higher premiums for those who remain. Actuaries estimate a 7% to 11.5% increase in 2027 for those still in the ACA system, further pressuring insurers and consumers alike. With open enrollment closing on January 15 in most states, the window for action is shrinking, and many are left with difficult choices.
What This Means for the Health Insurance Market and Investors
From a financial perspective, the ACA's struggles highlight growing concerns about healthcare affordability and consumer behavior. As more people drop coverage or switch to cheaper plans, insurers are facing a double challenge: higher costs for those who remain in the risk pool and the potential for fewer enrollees overall. This dynamic could pressure health insurance companies' profitability and stock valuations, especially if the trend continues into 2027 as projections show.
For investors, the key takeaway is that the ACA's financial viability remains tied to policy decisions in Washington. The Senate failed to pass bills to extend enhanced subsidies, and with no new legislation on the horizon, the market is bracing for more volatility. That means investors should keep an eye on enrollment numbers, premium changes, and any signs of regulatory shifts. If the ACA continues to lose market share, alternative coverage options — or even a shift to employer-sponsored plans — could become more attractive to consumers.
Looking Ahead: Policy Uncertainty and Consumer Behavior Shifts
The uncertainty around ACA subsidies and premiums isn't just a 2026 issue — it's shaping the long-term trajectory of healthcare in America. With more people opting for high-deductible plans or going without coverage altogether, the risk of financial strain for individuals grows, while the broader health insurance market faces pressure to adapt. For now, the focus is on the December 15 deadline as noted, but the larger question remains: how sustainable is the current model of ACA coverage?
As we move into 2026 and beyond, the ACA's future will likely be shaped by a combination of policy changes, consumer behavior, and market forces. Investors should watch for shifts in enrollment trends, especially as data for 2027 premiums start to emerge. If the risk pool continues to shrink, the cost burden on those who remain could become unsustainable, leading to more calls for reform. At the end of the day, the ACA is a key pillar of the U.S. healthcare system — and its challenges are far from over.
Delivering real-time insights and analysis on emerging financial trends and market movements.
Latest Articles
Stay ahead of the market.
Get curated U.S. market news, insights and key dates delivered to your inbox.



Comments
No comments yet