Healthcare Cost Shifts: Spotting Undervalued Insurance Stocks in a Rising Expense Landscape
The relentless rise of healthcare costs has forced employers to rethink their benefits strategies, with a growing emphasis on shifting costs to employees through higher deductibles and out-of-pocket expenses. For investors, this presents a unique opportunity to identify insurers positioned to thrive in this environment. Companies with robust networks, scalable high-deductible health plans (HDHPs), and telehealth integration stand to benefit as employers prioritize affordability while maintaining access to care. Let's dissect the trends and uncover undervalued stocks poised for growth.
The Employer Cost-Shifting Playbook: Key Trends
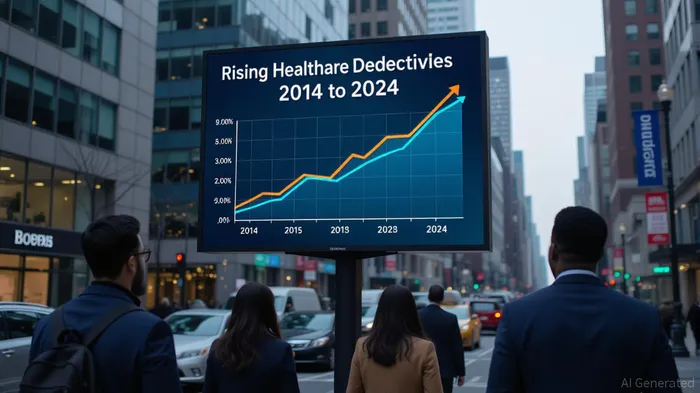
Recent surveys, including the 2024 Kaiser Family Foundation Employer Health Benefits Survey, reveal a clear pattern: deductibles are here to stay. The average single-coverage deductible rose to $1,787 in 2024, 47% higher than a decade ago, with 32% of workers facing deductibles of $2,000 or more. Meanwhile, employers are adopting strategies like self-funded plans (63% of workers now enrolled) to gain control over cost structures, often paired with telehealth tools to manage utilization.
The GLP-1 drug dilemma adds complexity. While only 18% of large firms broadly cover these medications for weight loss, rising demand is straining budgets. Insurers with strong pharmacy benefit management (PBM) capabilities or cost-sharing tools could capitalize on this tension by offering solutions to mitigate drug expenses.
Why Insurers Are Key Players in This Shift
Employers are increasingly looking for partners that can balance affordability and quality. Insurers that excel in the following areas are likely to outperform:
1. HDHP and HSA Integration: Plans like HDHPs, which pair high deductibles with health savings accounts (HSAs), are gaining traction. Insurers with strong administrative infrastructure to manage HSAs and attract younger, healthier populations will see demand surge.
2. Telehealth and Digital Tools: Employers are expanding virtual care options to reduce costs and improve access. Insurers with built-in telehealth platforms or partnerships (e.g., with Castlight Health) can reduce unnecessary in-person visits.
3. Self-Funded Plan Management: Third-party administrators (TPAs) that handle self-funded plans—often for large employers—can generate steady revenue streams.
4. Pharmacy Benefit Management: Controlling drug costs, particularly for high-cost therapies like GLP-1s, is critical. PBMs with transparent pricing and formulary expertise will be in demand.
Top Stocks to Watch
1. UnitedHealth Group (UNH)
Why it's a winner: UnitedHealth's Optum division dominates the PBM and telehealth spaces, with OptumRx managing $130 billion in drug claims annually. Its self-funded plan offerings, including the Optum Self-Funded Solutions platform, cater to employers seeking cost control. Optum's Care Management programs also address chronic conditions, aligning with employers' focus on prevention.
UNH has underperformed the S&P 500 in recent years, creating a potential buying opportunity as its diversified offerings gain traction in cost-conscious markets.
2. Cigna (CI)
Why it's a winner: Cigna's TPA business, which manages self-funded plans for large employers, grew by 7% in 2023. Its telehealth platform, CignaCI-- Virtual Care, integrates with employer networks, reducing costs while expanding access. CI's focus on mental health and work-life benefits (e.g., employee assistance programs) also aligns with trends like the 48% of large firms expanding mental health resources.
3. Anthem (ANTM)
Why it's a winner: Anthem's value-based care initiatives and strong regional networks (e.g., in California and the Midwest) provide cost efficiencies for employers. Its partnership with Centivo, a TPA provider, strengthens its self-funded offerings. Anthem's recent price-to-book ratio of 1.3x suggests undervaluation compared to peers trading at 1.6x or higher.
4. Humana (HUM)
Why it's a winner: HUM's Medicare Advantage dominance is well-known, but its employer segment is quietly growing. The company's partnership with Livongo (now part of Teladoc) integrates chronic disease management tools, appealing to employers targeting cost-sensitive employees.
Risks and Considerations
- Regulatory headwinds: Policymakers may push to cap deductibles or mandate drug price transparency, which could disrupt cost-sharing strategies.
- Employer pushback: Overly aggressive cost-shifting could reduce employee satisfaction, leading to retention issues. Insurers with poor member experience metrics (e.g., low HMO satisfaction scores) may struggle.
- Economic sensitivity: A recession could force employers to cut benefits further, squeezing insurer margins.
ETF Play for Diversification
For investors seeking broad exposure, the Healthcare Select Sector SPDR Fund (XLV) offers a low-cost way to bet on the sector. XLV holds UNH (14%), CI (8%), and ANTM (6%), providing diversified exposure to the trends discussed.
Conclusion: Act on the Shift, but Stay Selective
The healthcare cost crisis is here to stay, and insurers with the right tools to navigate employer demands are set to profit. UnitedHealth Group (UNH) stands out as a top pick for its PBM and telehealth strengths, while Cigna (CI) and Anthem (ANTM) offer compelling valuations in their niches. Investors should pair these picks with a watch on XLV for sector momentum. However, stay cautious of regulatory risks and monitor employer surveys for shifts in benefit design. The next phase of healthcare cost management will reward insurers that blend affordability with innovation—act before the market catches on.
Tracking the pulse of global finance, one headline at a time.
Latest Articles
Stay ahead of the market.
Get curated U.S. market news, insights and key dates delivered to your inbox.

Comments
No comments yet