New York's Medicaid Rollback: Coverage Gaps, Fiscal Strains, and Policy Uncertainty
The federal shift codified in H.R.1 will slash New York's Essential Plan funding by $7.5 billion annually, directly threatening health coverage for 1.7 million low- and middle-income residents. According to the federal funding report, while the state plans to maintain coverage for 1.3 million enrollees under a Basic Health Program, 450,000 individuals will lose their zero-premium plans. This reversal undermines the 2024 expansion that had provided comprehensive, no-cost insurance to residents at 250% of the Federal Poverty Level (FPL), erasing their average annual savings of $6,000 per person.
This policy change compounds existing enrollment instability. Nationally, Medicaid/CHIP enrollment has fallen 31% from its March 2023 peak, with procedural issues responsible for 69% of disenrollments as of June 2025. New York, despite higher retention rates from its ACA expansion, likely faces similar challenges with coverage stability for families renewing plans. The loss of zero-premium coverage increases uncompensated care costs and threatens local provider sustainability, particularly in communities already strained by reduced healthcare spending.
The July 2026 effective date creates a transition window where coverage uncertainty could deter routine care among vulnerable groups. Low- and middle-income households, especially those near the 250% FPL threshold, face immediate financial pressure, while rural clinics risk closure from lost patient volume and revenue. Procedural disenrollment hurdles may further delay assistance for those navigating the shift, compounding the policy's impact on healthcare access for New York's most economically vulnerable residents.
Economic Ripple Effects & State Fiscal Risks
The proposed federal cuts to Medicaid and SNAP would trigger significant macroeconomic consequences, straining state budgets and household stability. The "One Big Beautiful Bill" plan proposes $863 billion in Medicaid and $295 billion in SNAP cuts over a decade. This would slash spending for low-income households through work requirements, 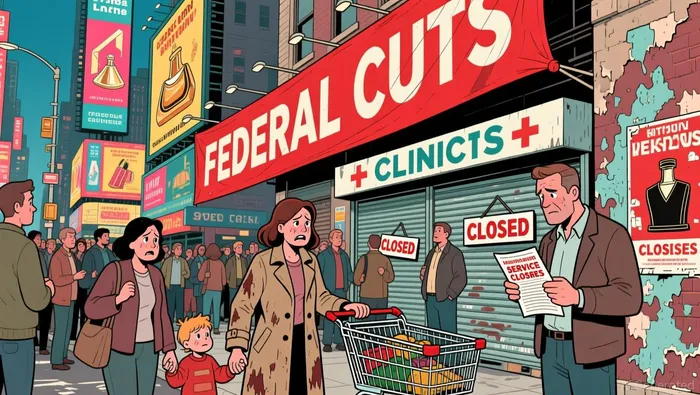 benefit reductions, and eligibility restrictions, ultimately causing 1.2 million job losses and a 0.8% increase in unemployment by 2029. States would collectively lose $154 billion in gross domestic product and $12.2 billion in tax revenues as a direct result, with higher-poverty states facing disproportionate harm. These cuts combine with anticipated coverage losses from Affordable Care Act marketplace changes, risking 16 million more uninsured Americans by 2034.
benefit reductions, and eligibility restrictions, ultimately causing 1.2 million job losses and a 0.8% increase in unemployment by 2029. States would collectively lose $154 billion in gross domestic product and $12.2 billion in tax revenues as a direct result, with higher-poverty states facing disproportionate harm. These cuts combine with anticipated coverage losses from Affordable Care Act marketplace changes, risking 16 million more uninsured Americans by 2034.
The loss of federal Medicaid funding would particularly strain state finances and healthcare systems. States relying heavily on Medicaid matching funds would absorb significant budget shortfalls, directly reducing resources available for other public services. Healthcare providers would face steep declines in patient volume and revenue, threatening their operational sustainability. Uncompensated care costs for hospitals and clinics, already a burden referenced qualitatively in prior analysis, would likely surge as vulnerable populations lose coverage without alternative payment sources. This fiscal pressure on providers could further reduce access to care, especially in underserved rural and urban areas.
Implementation uncertainty casts a shadow over these projections. The sheer scale of the proposed cuts faces considerable political and legal hurdles. Work requirements and eligibility restrictions could prove difficult to enforce nationwide, while legal challenges might limit the bill's immediate impact. States may also attempt to mitigate the effects through supplemental funding or policy adjustments, though resources are already constrained. The actual economic damage hinges on the final enacted legislation and its effective date, meaning the $154 billion GDP loss and $12.2 billion tax revenue decline remain long-term forecasts rather than imminent certainties.
Compliance Challenges & ROI Guardrails
Regulatory uncertainty remains a significant headwind for Medicaid-focused ROI projections. While North Carolina demonstrated relative enrollment stability by expanding eligibility pathways, New York faces heightened vulnerability under recent federal changes. The House-passed budget bill, analyzed by the Congressional Budget Office, could trigger massive coverage disruptions: 11 million Americans might lose Medicaid coverage and 5 million could lose ACA subsidies, totaling 16 million affected individuals. These losses disproportionately strain low-income households, with CBO estimating a 4% depletion of their resources due to program cuts. This fiscal pressure could erode household spending power and increase uncompensated care burdens on New York hospitals.
The 2025 federal budget reconciliation law, signed by President Trump, introduces critical compliance variables. It modifies eligibility rules and funding structures for Medicaid and subsidies, creating operational friction for states like New York. While the law's broad strokes are clear, its precise implementation timeline and state-specific financial impacts remain uncertain, requiring vigilant monitoring. States with larger pre-expansion populations, like New York, face compounded risks as procedural disenrollments-driven primarily by administrative hurdles rather than eligibility changes-continue to challenge coverage continuity. These unresolved renewal challenges directly threaten the stability of state budgets and the long-term ROI projections for healthcare providers serving Medicaid populations.
Providers must therefore stress-test their models against multiple scenarios. The potential $864 billion federal cut to Medicaid represents a structural shift, not a temporary fluctuation. Coupled with the projected 4% resource loss for low-income households, this creates a feedback loop: reduced consumer health spending, increased emergency room utilization, and slower revenue growth for safety-net hospitals. Compliance costs associated with navigating new eligibility rules and managing enrollment volatility will further compress margins. Stakeholders should prioritize tracking New York's specific enrollment retention rates and federal implementation guidance, as these variables will determine whether current ROI models hold under the new legislative framework.



Comentarios
Aún no hay comentarios