Geopolitical and Ethical Risks in Global Healthcare Infrastructure Funding: Assessing the Long-Term Financial Implications of Regulatory Scrutiny on World Bank-Backed Projects
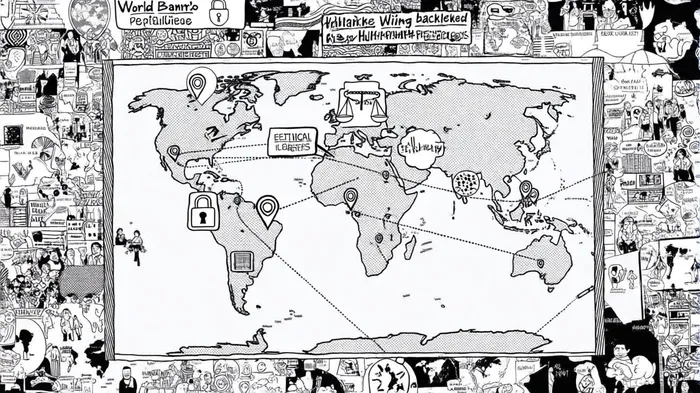
The World Bank's ambitious goal to expand healthcare access to 1.5 billion people by 2030[1] faces mounting challenges from regulatory scrutiny, geopolitical tensions, and ethical dilemmas. These factors are reshaping the financial viability of its infrastructure projects, particularly in low- and middle-income countries (LMICs). As global health financing shifts toward sustainable, country-led models[4], the interplay between policy changes, geopolitical dynamics, and ethical concerns is creating a complex landscape for long-term investment.
Regulatory Scrutiny and Financial Implications
Recent regulatory changes in healthcare, particularly in the U.S., have cascading effects on global projects. The Centers for Medicare & Medicaid Services (CMS) introduced value-based care models, including prepaid shared savings for Accountable Care Organizations (ACOs) and a revised Physician Fee Schedule[5]. While these aim to reduce costs domestically, they indirectly strain World Bank-funded systems in LMICs by altering global funding flows. For example, U.S. Medicaid funding reductions and stricter eligibility criteria could shift the payer mix in partner countries, increasing uncompensated care and diverting resources from infrastructure development[3].
Cybersecurity mandates, such as the U.S. Department of Health and Human Services' (HHS) requirement for mandatory encryption of electronic health data[5], add operational costs. World Bank-backed digital health platforms—like Panama's Telemedicine Program, which served 60,000 patients with chronic diseases between 2021 and 2023[2]—now face higher compliance burdens. These costs could erode budgets allocated for infrastructure, forcing trade-offs between technology upgrades and facility expansion.
Geopolitical Risks and Funding Uncertainty
Geopolitical tensions are compounding financial risks. The World Bank's Pandemic Fund, designed to address global health preparedness, has been criticized for opaque governance and misaligned aid allocation[1]. With an estimated $10.5 billion needed annually, the fund's insular design risks underperformance, undermining trust among donor and recipient nations. This mirrors broader challenges in global health financing, where fragmented aid and shifting donor priorities create instability[5].
Case studies highlight these risks. In Uganda and the Philippines, World Bank-funded hospitals under the International Finance Corp. (IFC) faced allegations of detaining patients until they could pay bills and denying emergency care to those without financial capacity[2]. These incidents not only damaged reputations but also triggered regulatory reviews, leading to delayed disbursements and increased oversight costs. Geopolitical dynamics further complicate matters: U.S. influence over World Bank decisions and the institution's alignment with neoliberal economic principles have drawn criticism for prioritizing financial returns over equitable outcomes[5].
Ethical Challenges and Systemic Inequities
Ethical concerns are deeply intertwined with financial outcomes. Performance-based financing (PBF) initiatives, which tie payments to health outcomes, have shown limited effectiveness in under-resourced systems. A World Bank blog post noted that PBFPBF-- often incentivizes inappropriate care and fails to address structural gaps like drug shortages[1]. In Ethiopia and Indonesia, locally driven reforms supported by the Bank have succeeded, but these projects require sustained investment in domestic health financing—a challenge when global priorities shift[4].
Moreover, research funding for global health often reflects the priorities of high-income countries rather than the needs of LMICs[5]. This misalignment perpetuates systemic inequities, as LMICs lack the capacity to independently produce vaccines or medicines. For instance, the World Bank's focus on digital health solutions in Latin America—such as seismic-resistant hospitals in Sint Maarten and renewable energy systems in Haiti[2]—has improved infrastructure but does little to address root causes of health disparities.
Long-Term Financial Implications
The cumulative effect of these challenges is a recalibration of funding models. The World Bank's shift from fragmented aid to country-led financing[4] is a step toward sustainability, but it requires navigating regulatory and geopolitical headwinds. For example, U.S. tariffs on medical supplies and potential cuts to NIH grants could raise costs for hospitals in partner countries[3], while geopolitical tensions may deter private-sector participation in public-private partnerships (PPPs)[3].
A 2025 World Bank report underscores the need for resilient health systems that integrate climate-smart infrastructure and digital solutions[2]. However, achieving this vision demands not only financial resources but also political will to address ethical and governance issues. The Bank's collaboration with ministries of finance and health to improve budget execution—highlighted in a joint WHO-World Bank report[5]—offers a blueprint for aligning funding with UHC goals.
Conclusion
The World Bank's healthcare initiatives are at a crossroads. While regulatory scrutiny and geopolitical risks pose significant financial challenges, they also highlight opportunities for innovation. By prioritizing transparency, local ownership, and ethical alignment, the Bank can mitigate risks and ensure sustainable progress toward universal health coverage. However, without addressing systemic inequities in global health financing, the long-term success of these projects remains uncertain.



Comentarios
Aún no hay comentarios