Centene's Guidance Withdrawal: A Systemic Crack in Managed Care Models?
The healthcare insurance sector has long relied on precise actuarial models to predict morbidity trends, manage risk-adjustment transfers, and set premium rates. But CenteneCNC-- Corporation's abrupt withdrawal of its 2025 earnings guidance—driven by a $1.8 billion shortfall in risk-adjustment revenue and soaring Medicaid costs—has exposed a critical vulnerability in these models. This move raises urgent questions: Are Centene's struggles an isolated misstep, or do they signal a broader industry reckoning with flawed assumptions about risk, cost inflation, and regulatory stability? For investors, the answer demands a reevaluation of valuation multiples and a shift toward defensive strategies in an increasingly volatile sector.
The Centene Crisis: A Confluence of Risks
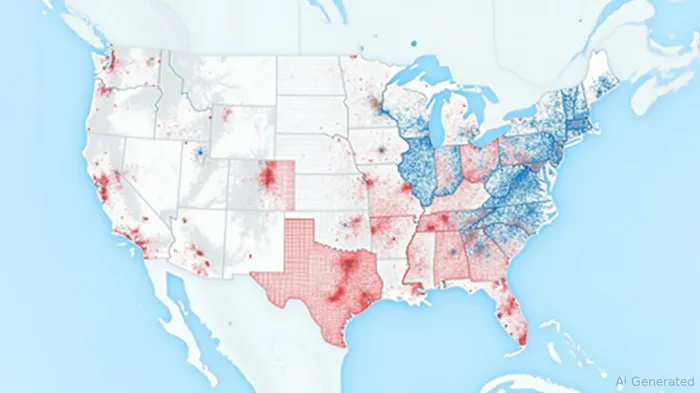
Centene's withdrawal stems from two interconnected challenges. First, its Marketplace business faced a catastrophic mismatch between projected and actual member health profiles. The risk-adjustment mechanism, which redistributes funds to insurers with sicker populations, backfired: Centene's risk pool proved far costlier than anticipated, costing $2.75 in adjusted EPS. Second, Medicaid costs surged in key states like New York and Florida, driven by behavioral health, home care, and specialty drugs. These pressures pushed Medicaid's Health Benefits Ratio (HBR)—the proportion of revenue spent on medical care—higher in Q2 2025, squeezing margins.
But these issues are not unique to Centene. The Medicaid program's state-by-state variability creates systemic risks: rising utilization of high-cost services outpaces rate increases in many regions, leaving insurers with inadequate reimbursement. Meanwhile, the Marketplace's reliance on risk adjustment has always been fragile, as accurate morbidity forecasting requires near-perfect data—a tall order in a dynamic population.
Industry-Wide Implications: Valuation at Risk
Investors have historically rewarded healthcare insurers with high valuation multiples, assuming stable underwriting and predictable revenue streams. But Centene's crisis undermines this premise. If Medicaid cost trends and Marketplace morbidity are harder to model than previously believed, growth forecasts for insurers with heavy exposure to these segments—such as Molina HealthcareMOH-- or Kaiser Permanente—could be overly optimistic.
Consider the math: A single $1 billion risk-adjustment shortfall (like Centene's) can slice ~$1.50 off EPS for a $10 billion insurer. If similar gaps emerge industrywide, valuation multiples for the sector could contract sharply. Current median price-to-earnings ratios for Medicaid-focused insurers (e.g., ~12x) may overstate resilience if margins compress further.
Investment Strategy: Defense Over Aggression
The lesson is clear: Avoid insurers overly reliant on volatile segments and favor those with structural advantages. Three actionable strategies emerge:
Favor Medicare Advantage Dominance:
Centene's strong Medicare Advantage performance (and the sector's steady growth) highlights a safer harbor. Medicare's predictable reimbursement and lower morbidity variability make it less exposed to the same risks. Firms like HumanaHUM-- and UnitedHealthcare, with leading Medicare Advantage platforms, offer steadier returns.Prioritize Medicaid Rate-Adjustment Mechanisms:
States like Florida and New York are gradually raising Medicaid rates to match rising costs, but not all insurers benefit equally. Companies with strong lobbying power or geographically concentrated footprints—such as WellCare Health Plans in Florida—may secure better rate hikes, shielding margins.Avoid High-Marketplace Exposure:
The Marketplace's risk-adjustment model is a double-edged sword. Insurers with large, geographically dispersed populations (e.g., Anthem or Cigna) face heightened volatility. Investors should steer clear until these companies demonstrate better underwriting discipline or diversify into more stable lines.
Conclusion: A Sector Divided
Centene's withdrawal is a wake-up call. The managed care model's assumptions about cost predictability and risk management are fraying. For investors, this means a bifurcated landscape: defensive insurers with Medicare strength or Medicaid rate leverage will outperform those betting on unstable segments. The era of one-size-fits-all valuation multiples is over. In this new reality, precision—not aggression—is the key to navigating healthcare insurance's choppy watersWAT--.
Investment Takeaway: Reduce exposure to insurers with heavy Marketplace or Medicaid-only portfolios. Focus on firms with Medicare Advantage scale, geographic Medicaid rate advantages, or diversified risk profiles. The sector's next phase will reward caution—and punish overreach.


Comentarios
Aún no hay comentarios